Preparation and administration for WINREVAIR (sotatercept-csrk)
Administration is subject to monitoring of hemoglobin (Hgb) and platelet count.
WINREVAIR is intended for use under the guidance of a healthcare professional. Patients and caregivers may administer WINREVAIR when considered appropriate and when they receive training and follow-up from the healthcare provider on how to reconstitute, prepare, measure, and inject WINREVAIR.
Confirm at subsequent visits that the patient and/or caregiver can correctly prepare and administer WINREVAIR, particularly if the dose changes or the patient requires a different kit.
Refer to the Instructions for Use (IFU) for detailed instructions on the proper preparation and administration of WINREVAIR.
Instructions for Use videos are available
You can access the Instructions for Use (1-vial kit, 2-vial kit) videos for WINREVAIR here.
Selecting the appropriate product kit
If a patient’s body weight requires the use of two 45-mg vials or two 60-mg vials of lyophilized product, use a 2-vial kit instead of two individual 1-vial kits. A 2-vial kit includes instructions to combine the contents of two vials, which aids in measuring the proper dosage and eliminates the need for multiple injections.
1-vial kits
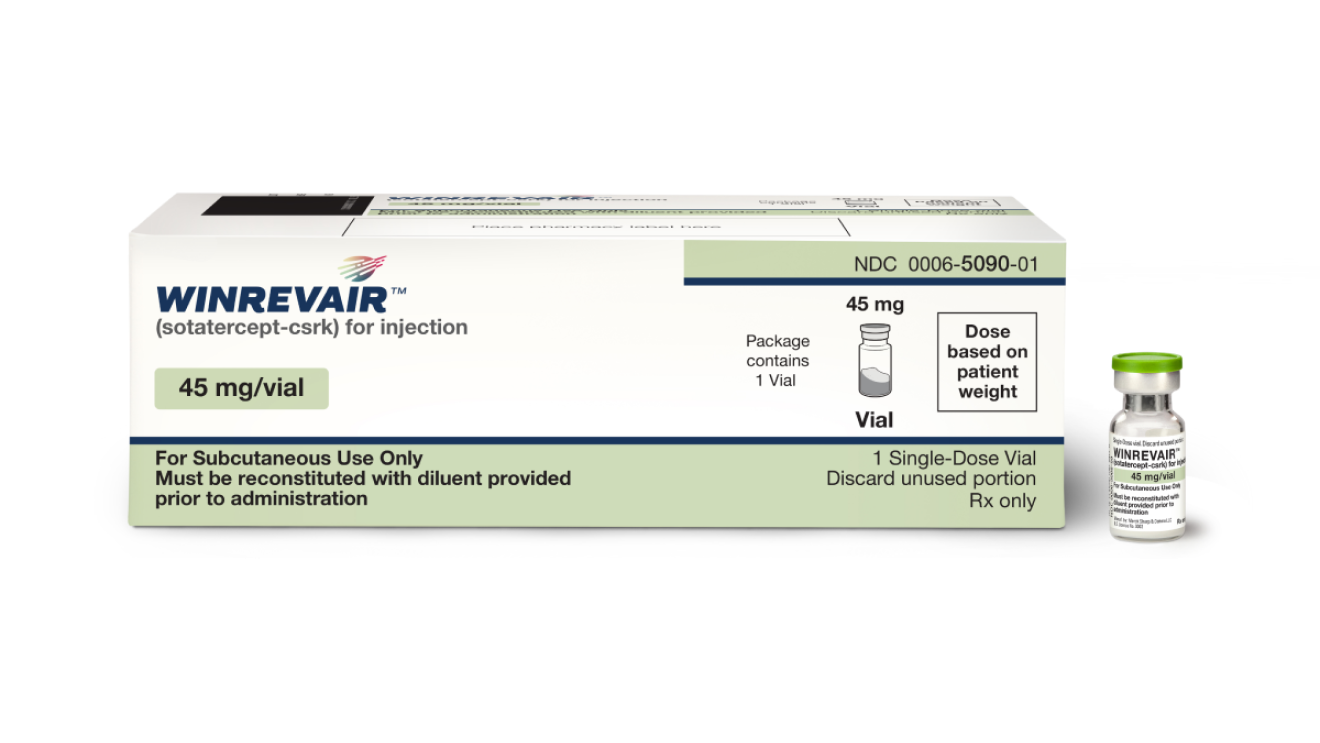
45 mg kit (containing 1 x 45 mg vial)
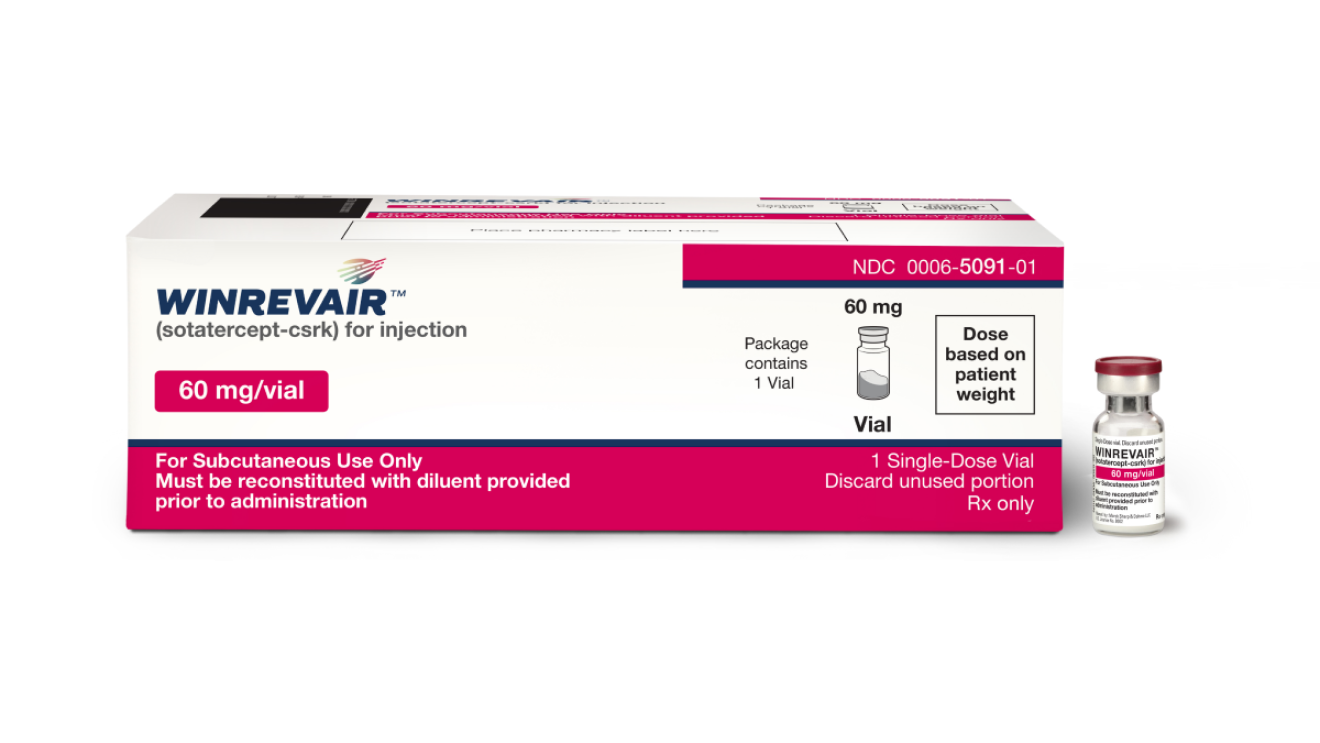
60 mg kit (containing 1 x 60 mg vial)
2-vial kits
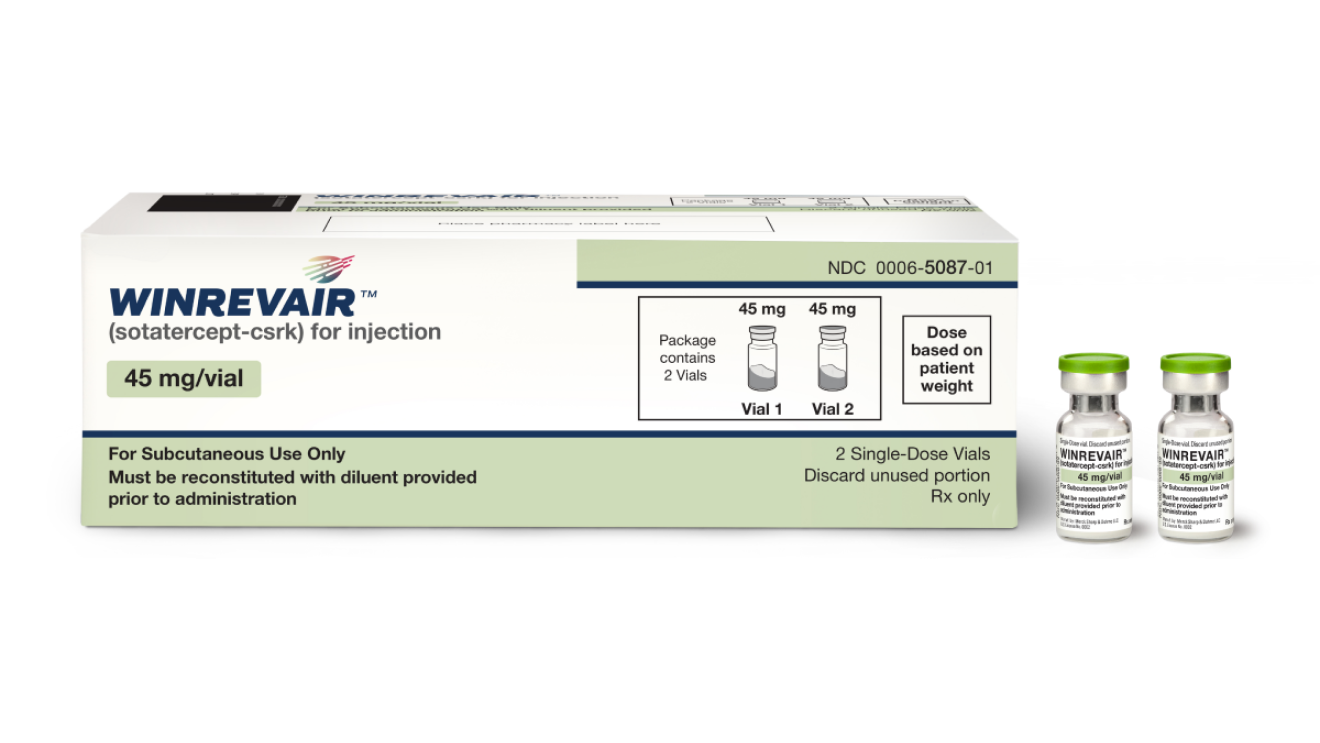
90 mg kit (containing 2 x 45 mg vials)
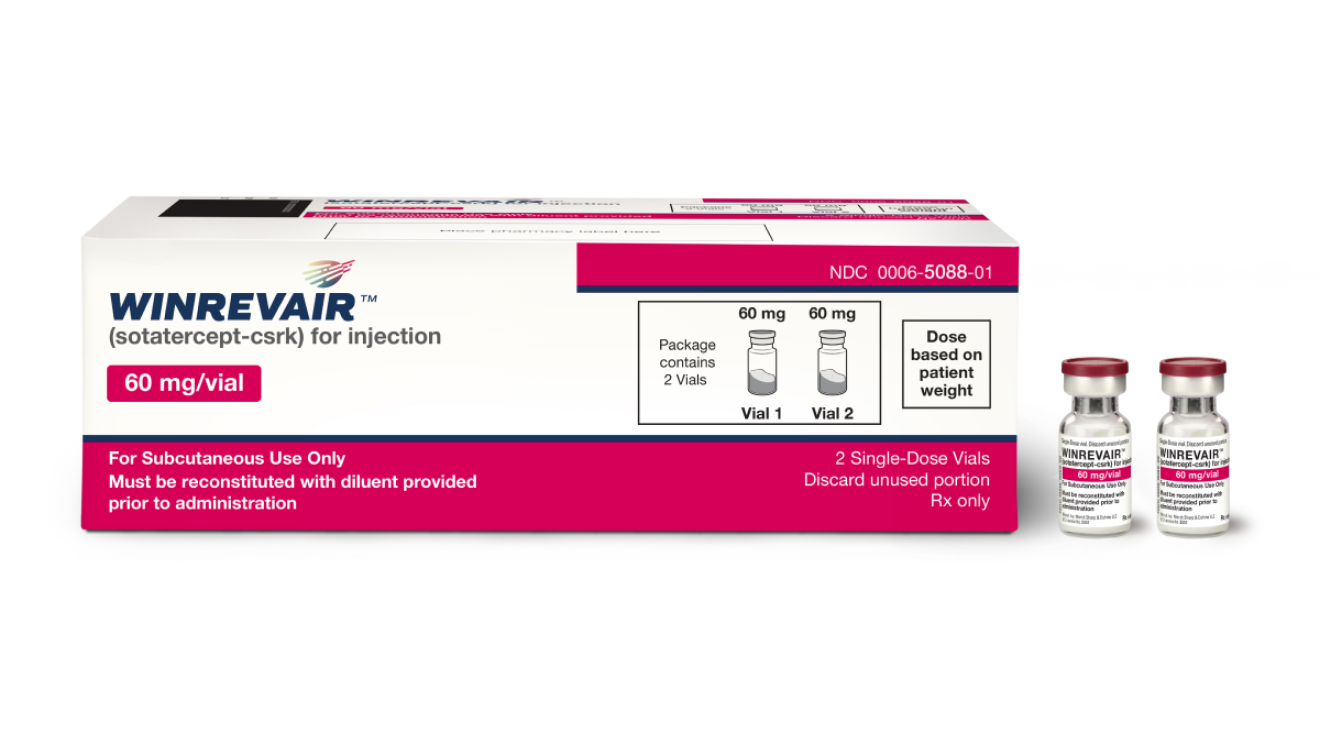
120 mg kit (containing 2 x 60 mg vials)
Not actual size.
Reconstitution instructions
- Remove the injection kit from the refrigerator and wait 15 minutes to allow the pre-filled syringe(s) and drug product to come to room temperature prior to preparation.
- Attach the vial adapter to the vial.
- Visually inspect the pre-filled syringe for any damage or leaks and the Sterile Water for Injection inside to ensure there are no visible particles.
- Snap off the cap of the pre-filled syringe and attach the syringe to the vial adapter.
- Inject all of the Sterile Water for Injection from the attached syringe into the vial containing the lyophilized powder. This will provide a final concentration of 50 mg/mL.
- Gently swirl the vial to reconstitute the drug product. DO NOT shake or vigorously agitate.
- Allow the vial to stand for up to 3 minutes to allow bubbles to disappear.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- When properly mixed, WINREVAIR should be clear to opalescent and colorless to slightly brownish-yellow and does not have clumps or powder.
- If prescribed a 2-vial presentation, repeat the steps within this section to prepare the second vial.
- Use the reconstituted solution as soon as possible, but no later than 4 hours after reconstitution. Discard unused reconstituted solution.
Syringe preparation
- Turn the syringe and vial upside-down and withdraw the appropriate volume for injection, based on the patient’s weight.
- If the dose amount requires the use of two vials, withdraw the entire contents of the first vial and slowly transfer full contents into the second vial.
- Turn the syringe and vial upside-down and withdraw the required amount of drug product.
- If necessary, remove excess drug product.
- If necessary, remove excess air from the syringe.
Administration instructions
WINREVAIR is for subcutaneous injection.
- Select the injection site on the abdomen (at least 2 inches away from navel), upper thigh, or upper arm, and swab with an alcohol wipe. Select a new site for each injection that is not scarred, tender, or bruised.
- For administration by the patient or caregiver, use only the abdomen and upper thigh (see IFU).
- Perform subcutaneous injection.
